Weight loss injections have become a popular option for individuals looking to manage their weight with medical support. These treatments can help those struggling to achieve healthier weight goals, particularly when diet and exercise alone are not enough. However, while body mass index is useful, understanding its limitations is essential when considering medical options.
This article explains the connection between BMI and weight loss injections, highlighting how they can work together to support better health outcomes. By examining the science, benefits, and risks, you’ll gain clarity on whether these treatments could be the right choice for you.
What is BMI and Why Does it Matter?

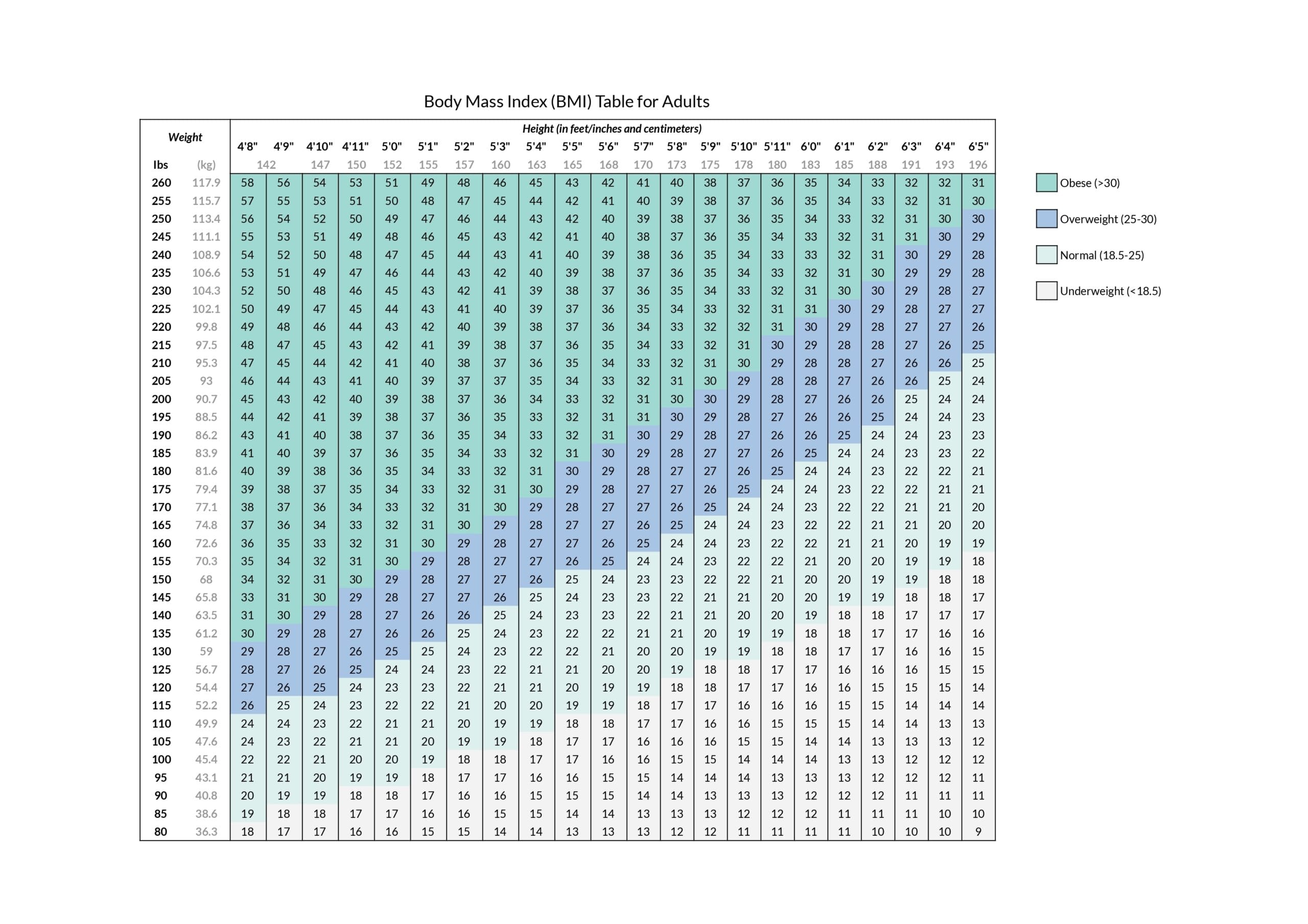
Body Mass Index, or BMI, is a widely used calculation that helps assess whether an individual’s weight falls within a healthy range. It is determined by dividing a person’s weight in kilograms by the square of their height in metres. This simple formula provides a numeric value that classifies weight, such as underweight, healthy, overweight, or obese.
The BMI scale serves as a guide to understanding the potential health risks associated with weight. For example, a higher BMI often correlates with an increased risk of conditions like type 2 diabetes, heart disease, and certain cancers. A BMI below the healthy range may indicate potential nutritional deficiencies or other health concerns.
While this is a helpful tool, it’s not without its limitations. It doesn’t account for factors such as muscle mass, bone density, or body composition. For this reason, healthcare professionals often use BMI alongside other measures, such as waist circumference or medical history, to build a more complete picture of an individual’s health.
The Connection Between BMI and Weight Loss Treatments

BMI plays a key role in identifying individuals who may benefit from medical weight loss treatments, including injections. Healthcare providers often use BMI for weight loss thresholds to determine whether someone is eligible for these interventions. The thresholds are guided by medical research linking higher BMI values to increased health risks.
By focusing on BMI, healthcare providers aim to target treatments where they are most likely to improve overall health. BMI for weight loss injections, in particular, are often recommended for those who struggle with traditional weight management methods and meet specific BMI criteria.
In this context, BMI serves as a useful benchmark for creating personalised treatment strategies. However, it’s worth noting that healthcare providers don’t rely solely on BMI. Factors like comorbidities, lifestyle, and overall health are also considered before recommending weight loss treatments.
How BMI Determines Eligibility for Weight Loss Injections

Typically, these treatments are recommended for individuals with a BMI of 30 or above, categorised as obese. For those with a BMI of 27 or higher, weight loss injections may also be an option if they have obesity-related health conditions such as type 2 diabetes or hypertension.
However, BMI is only part of the evaluation process. Healthcare professionals assess a person’s overall health, considering factors such as medical history, lifestyle, and the presence of other conditions. Comorbidities, like high blood pressure or sleep apnea, often play a significant role in determining whether these treatments are suitable.
A personalised consultation is essential to ensure the treatment is safe and effective. During this process, healthcare providers evaluate each individual’s unique circumstances, offering more ways to achieve effective weight management beyond BMI alone.
How Weight Loss Injections Aid in BMI Reduction

Weight loss injections, such as GLP-1 agonists like semaglutide, work by mimicking hormones that regulate appetite and blood sugar levels. These treatments help reduce hunger, slow digestion, and promote a feeling of fullness, leading to lower calorie intake. Over time, this process can lead to significant weight loss and a reduction in BMI.
In addition to appetite control, these injections may improve metabolism, helping the body use energy more efficiently. Clinical studies have shown that consistent use of weight loss injections can result in noticeable reductions in BMI, particularly when combined with healthy lifestyle changes.
However, for the best results, these treatments should be part of a broader weight loss plan. Incorporating a balanced diet, regular exercise, and ongoing medical supervision increases the effectiveness of weight loss injections and provides sustainable progress.
Benefits of Using BMI to Guide Weight Loss Treatment

BMI offers a straightforward way to determine eligibility for weight loss treatments like injections. By setting clear thresholds, it simplifies the process of identifying individuals who could benefit most from medical support. This can be especially helpful for healthcare providers when creating standardised treatment plans.
Additionally, BMI serves as a measurable way to track progress over time. As weight loss treatments take effect, reductions in BMI can provide motivation and a tangible sense of achievement for patients. This clarity helps individuals stay focused on their goals.
Beyond its practical use, BMI helps establish consistency in treatment approaches, ensuring that interventions are targeted at those with the greatest need. While it has its limitations, BMI remains a valuable starting point in creating personalised strategies for better health outcomes.
Potential Risks of Weight Loss Injections Based on BMI
While weight loss injections can be effective, they are not without risks. Side effects such as nausea, diarrhoea, or fatigue are relatively common, particularly in the early stages of treatment. For some individuals, these symptoms may impact their ability to stick with the therapy.
Another concern is the potential for over-reliance on BMI as the sole measure of health. BMI does not account for factors like muscle mass, body composition, or individual differences, which means it might not always provide a complete picture of someone’s health. This could lead to treatments being prescribed when other approaches might be more suitable.
Misuse of these injections, such as using them without proper medical supervision, can pose additional risks. It’s advised for individuals to work closely with healthcare professionals who can monitor their progress and that the treatment is both safe and effective.
Is Combining BMI Monitoring and Injections Right for You?
Deciding whether weight loss injections and BMI monitoring are suitable requires careful consideration. Consulting a healthcare professional is essential to evaluate your unique health profile, including any underlying conditions, lifestyle factors, and weight loss goals.
While BMI provides a helpful guideline for eligibility, it should be seen as just one part of a broader approach. Effective weight loss strategies often include a combination of medical treatment, dietary adjustments, regular physical activity, and emotional support.
It’s important to remember that everyone’s journey is different. Factors like long-term health, realistic expectations, and personal circumstances play a significant role in determining whether this combination is right for you. A personalised approach, guided by medical advice, offers the best chance for success.
BMI and weight loss injections are closely linked in creating effective weight management strategies. By using BMI as a guideline, healthcare professionals can identify individuals who may benefit most from these treatments while considering other health factors.
While weight loss injections can reduce BMI and improve health outcomes, they are most effective when combined with a broader approach, including diet, exercise, and ongoing medical support. It’s essential to view BMI as a starting point rather than the sole measure of health, ensuring that treatment decisions are well-informed and personalised.
If you’re considering weight loss injections, consult with us at WePrescribe to explore your options and receive tailored advice. With the right guidance, you can take steps towards achieving your health goals safely and sustainably.


