Understanding and accessing various forms of female contraception is important to women’s autonomy over their reproductive health.
This guide offers an in-depth look at the variety of female contraception options available today, from long-acting devices to daily pills and emergency solutions.
Accessing accurate information is the first step towards using contraceptive prescription medication.
We hope that in providing this information, we aim to help you make informed decisions that best suit your health, lifestyle, and plans.
What is Female Contraception?
These methods are designed to prevent unintended pregnancies.
They range from hormonal and barrier options to long-acting reversible contraceptives (LARCs) and emergency measures.
The purpose of contraception extends beyond the prevention of pregnancy; it allows women to plan their futures, control their bodies, and manage their health conditions with greater freedom.
The availability of multiple contraception options means that there’s likely a method that matches almost every woman’s needs and preferences.
However, choosing the right method involves understanding the differences between them, including how they work, their effectiveness, potential side effects, and how they fit into your lifestyle.
It’s important to challenge the misconceptions and stigmas that often surround female contraception.
Educating yourself and others about these options promotes a supportive environment where women can make choices about their reproductive health without fear or judgment.
Why is Female Contraception Important?
This plays an important role in enabling women to take control of their reproductive health, influencing their ability to pursue education, career goals, and personal aspirations without the interruption of an unplanned pregnancy.
Its importance extends to promoting choice, allowing women and couples to decide if and when they want to have children.
Beyond personal empowerment, accessibility has significant societal benefits. It contributes to reducing maternal and infant mortality rates by preventing unintended pregnancies, especially those that may pose health risks.
It also supports sustainable family planning and population growth, which are crucial for the socioeconomic development of communities.
Preventing sexually transmitted infections (STIs) in the case of barrier methods, and allowing women to plan their pregnancies, supports overall public health initiatives.
These broader implications highlight why ensuring women have access to sexual education and a range of contraceptive options is a public health priority.
Contraceptive Injection

The contraceptive injection is a method that administers hormones via injection to prevent pregnancy.
This method is known for its efficacy and convenience, offering protection for a duration ranging from one to three months, depending on the type.
One of the key advantages of the contraceptive injection is its long-term nature, which eliminates the need for daily attention, making it an appealing option for many women.
Like all of these methods, it has its drawbacks. Potential side effects can include changes in menstrual patterns, weight gain, and mood fluctuations.
Despite these considerations, the injection remains a popular choice for those seeking effective, longer-term contraception without the daily hassle.
Concerns regarding contraceptive injection often stem from misconceptions about its long-term effects on fertility and bone density.
It’s important to consult with a healthcare provider to understand the risks and benefits fully.
For women considering long-term use, discussing these aspects with a professional can help in making an informed decision that matches their health and reproductive goals.
Intrauterine System (IUS)

The intrauterine system (IUS) is a highly effective long-acting reversible contraceptive that is inserted into the uterus.
It releases hormones locally to prevent pregnancy and can remain in place for up to five years.
The IUS offers several benefits, including its ‘set and forget’ nature, making it a convenient option for women seeking long-term contraception without daily intervention.
There are both hormonal and non-hormonal IUS options available, catering to a wide range of preferences and medical considerations.
Hormonal IUS devices typically work by thickening the cervical mucus to prevent sperm from reaching the egg and thinning the lining of the uterus, which can also lead to lighter periods.
On the other hand, non-hormonal options, such as the copper IUD, create an environment that’s hostile to sperm.
Despite its high efficacy and convenience, the IUS may cause initial side effects like cramping or irregular bleeding.
Additionally, there are misconceptions about the risk of infection and the impact on future fertility.
It’s important to address these concerns with healthcare professionals to make sure that women have accurate information when considering this method.
Intrauterine Device (IUD)

The intrauterine device (IUD) is another form of long-acting reversible contraception that is inserted into the uterus to prevent pregnancy.
IUDs come in two main types: hormonal and copper-based (non-hormonal). The hormonal IUDs release a small amount of progestin, which works similarly to the hormonal IUS, while copper IUDs use copper’s spermicidal properties to prevent pregnancy.
IUDs are known for their longevity and efficacy, offering protection for up to 10 years depending on the type.
They are a preferred option for women looking for a long-term, reversible contraception method that doesn’t require daily management.
However, the process of inserting and removing an IUD requires a healthcare professional and can be uncomfortable for some women, which is an important factor to consider.
Misconceptions about IUDs, such as the increased risk of pelvic inflammatory disease or that they are only suitable for women who have already had children, have been largely debunked.
It’s essential to have a thorough consultation with a healthcare provider to discuss any potential risks and to determine whether an IUD is the right choice based on your medical history and lifestyle.
Combined Pill

The combined oral contraceptive pill, commonly known as the combined pill, is a widely used method of female contraception that contains synthetic forms of estrogen and progesterone.
Brands like Microgynon 30, Yasmin, and Rigevidon are among the options available.
The pill works by preventing ovulation, thickening cervical mucus to block sperm, and thinning the uterine lining to prevent a fertilised egg from implanting.
The combined pill offers several benefits beyond contraception, including regulating menstrual cycles, reducing menstrual pain, and alleviating acne.
Factors such as a history of blood clots, certain cancers, or smoking, especially in women over 35, may make the combined pill a less viable option.
One of the main advantages of the combined pill is its reversibility; fertility typically returns quickly after stopping the pill.
Missing doses can decrease its contraceptive efficiency, making understanding how to manage missed pills an important aspect of its use.
There are also misconceptions about the combined pill’s impact on long-term fertility and health.
While side effects can include nausea, weight gain, and mood changes, these typically diminish over time.
Discussing these factors with a healthcare provider can help determine if the combined pill is the right method for you, ensuring that your choice matches your health needs and lifestyle.
Progestogen-Only Pill (POP)
The progestogen-only pill (POP), with options like Cerazette and Cerelle, provides an alternative for women who cannot use estrogen-containing contraception.
POPs work mainly by thickening the cervical mucus, making it difficult for sperm to enter the uterus, and in some cases, by thinning the lining of the uterus or inhibiting ovulation.
POPs offer the advantage of being suitable for a wider range of women, including those who are breastfeeding or have certain health conditions that preclude the use of estrogen.
They are also reversible, with fertility returning shortly after the end of use.
However, they require strict rules for taking the pill at the same time every day, which is crucial for maintaining their effectiveness.
Common concerns about POPs include irregular menstrual bleeding, which can be a side effect as the body adjusts.
There’s also a belief that POPs are less effective than other forms of contraception, but when taken correctly, they are highly effective.
A healthcare provider can offer guidance on whether a POP is a suitable option and how to manage any side effects that may arise.
Emergency Contraception

In instances where regular contraception fails or in the absence of contraception during intercourse, emergency contraception offers a crucial second chance to prevent unintended pregnancy.
This category includes emergency contraceptive pills like the ellaOne morning after pill and Levonelle, as well as the copper IUD, which can be inserted up to five days after unprotected sex.
Emergency contraception pills work by delaying ovulation or making it difficult for a fertilised egg to implant in the uterus.
It’s important to note that these methods are for emergency use and are not intended as a regular form of contraception.
Their effectiveness depends on how quickly they are used after unprotected sex, with earlier use increasing the likelihood of preventing pregnancy.
Despite its importance, emergency contraception is surrounded by misconceptions, including unfounded concerns about its safety and long-term fertility effects.
It’s also wrongly thought to terminate an existing pregnancy, whereas it prevents pregnancy from occurring.
Clearing up these misunderstandings and providing accurate information about how to access emergency contraception is essential for ensuring women can make informed decisions in emergencies.
Consulting with a healthcare provider can provide personalised advice and clarify any concerns, ensuring that the choice of emergency contraception aligns with the individual’s needs and circumstances.
Contraceptive Patch

The contraceptive patch is a skin patch that releases a combination of estrogen and progestogen into the bloodstream, functioning similarly to the combined oral contraceptive pill.
Its main advantage is the convenience it offers; instead of daily administration, the patch is applied once a week for three weeks, followed by a patch-free week.
This method is particularly appealing for those who find it challenging to remember to take a pill every day.
The patch’s effectiveness is comparable to that of the combined pill, offering not only reliable contraception but also regulated menstrual cycles and reduced menstrual cramps for many users.
However, the patch may not be suitable for all women. Those with certain health conditions or risk factors, such as a history of blood clots or high blood pressure, may need to consider other contraception options.
Additionally, while rare, the patch can cause skin irritation or discomfort at the application site.
Addressing concerns and misconceptions about the contraceptive patch involves discussing its benefits and potential drawbacks with a healthcare provider.
They can guide the proper application and rotation of the patch sites to minimise skin irritation, ensuring a positive experience with this contraceptive method.
Contraceptive Implant
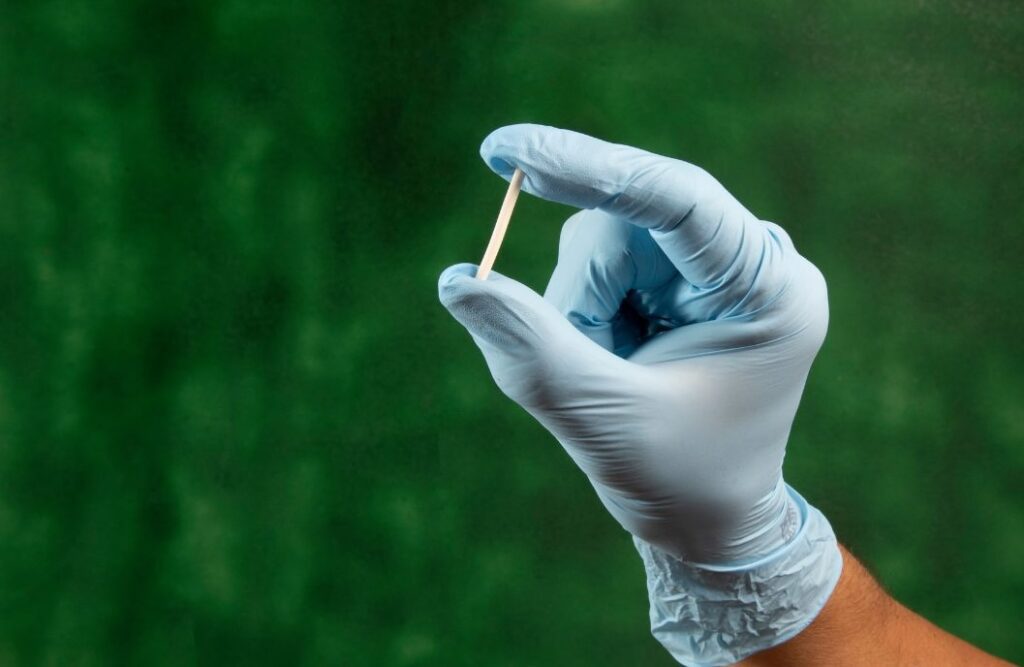
The contraceptive implant is a small, flexible rod that is inserted under the skin of the upper arm, where it releases progestogen to prevent pregnancy.
It’s one of the most effective methods available, with a success rate of over 99% and lasting up to three years.
One of the implant’s key advantages is its long duration of action, coupled with the fact that it doesn’t require daily management.
This makes it an excellent option for women seeking a hassle-free, long-term contraceptive solution.
The implant’s effects are also quickly reversible once removed, allowing for a quick return to fertility for those who wish to conceive.
However, potential side effects, such as irregular bleeding, can be a concern for some users.
There are misconceptions about the insertion process being painful and the implant affecting long-term fertility, both of which are generally unfounded.
Choosing the contraceptive implant involves considering your long-term reproductive health plans and lifestyle.
It’s crucial to consult with a healthcare provider to discuss the procedure, manage expectations regarding side effects, and ensure the implant is the right fit for your contraception needs.
Why is it Important You Choose the Right Contraception?
Choosing the right option is essential for ensuring satisfaction, adherence, and the best possible reproductive health outcomes.
With the vast amount of options available, it’s vital to consider personal preferences, lifestyle factors, and any health conditions that might influence the suitability of different methods.
Barriers to accessing and using contraception effectively can include misinformation, stigma, or limited healthcare resources.
Overcoming these barriers is important for personalised, informed contraceptive care.
Engaging in open discussions with healthcare providers, researching options, and considering long-term reproductive goals can help navigate this and find the most suitable method.
How Effective is Female Contraception?
The effectiveness of female contraception varies significantly among different methods, with factors such as adherence, method selection, and individual variability playing crucial roles.
Understanding the distinction between perfect use (how effective a method is when used exactly as directed) and typical use (how effective a method is in reality, accounting for human error) is key to setting realistic expectations about contraceptive efficacy.
For instance, long-acting reversible contraceptives (LARCs) like the IUD and implants boast higher effectiveness rates due to minimal user intervention.
In contrast, methods requiring daily attention, such as the oral contraceptive pill, might have lower effectiveness in typical use due to the possibility of missed doses.
Awareness of and communication about these variations in effectiveness can aid individuals in selecting the contraception method that best aligns with their lifestyle and capability for consistent use, thereby improving their contraceptive effectiveness.
Understanding and accessing the right female contraception options play a pivotal role.
The ability to choose from a variety of contraceptive methods empowers women to make decisions that best suit their health, lifestyle, and future aspirations.
As we work towards ensuring universal access to contraception and dismantling barriers to reproductive care, remember that resources like our video consultation are available to provide personalised advice and support.
Through education, advocacy, and compassionate healthcare, we can support each other in making informed choices about our bodies and futures, promoting a healthier, more empowered society.


